- HUMAN PROTEIN ATLAS SECTIONS
- TISSUE
- BRAIN
- SINGLE CELL TYPE
- TISSUE CELL TYPE
- PATHOLOGY
- IMMUNE CELL
- BLOOD PROTEIN
- SUBCELLULAR
- CELL LINE
- METABOLIC
|
|
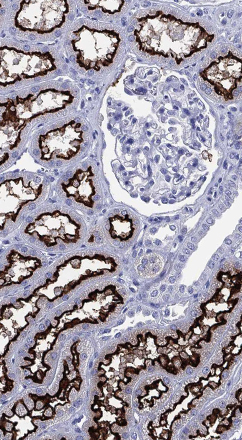
SARS-CoV-2The Human Protein Atlas (HPA) consortium is engaged in the corona epidemic in various ways to aid in the fight against the health consequences of this pandemic outbreak. The program involves both efforts to increase the knowledge-base of the disease and efforts to develop diagnostic tools and therapeutic drugs to combat the pandemic. In the following, published research papers involving HPA researchers are listed. Host-virus biology • F. Hikmet et al (2020) ”The protein expression profile of ACE2 in human tissues” Mol Syst Biol. 2020 16(7):e9610. • Carapito et al (2021) “Identification of driver genes for severe forms of COVID-19 in a deeply phenotyped young patient cohort” Science Translational Medicine, 10.1126/scitranslmed.abj7521 • Blixt et al (2021) “Covid-19 in patients with chronic lymphocytic leukemia: Clinical outcome and B- and T-cell immunity during 13 months in consecutive patients” Leukemia DOI: 10.1038/s41375-021-01424-w • Elfström et al (2021) “Differences in risk for SARS-CoV-2 infection among healthcare workers” Preventive Medicine Reports 24, 101518 • S. Havervall et al. (2021) "Robust humoral and cellular immune responses andlow risk for reinfection at least 8 months followingasymptomatic to mild COVID-19," Journal of Internal Medicine, Epub ahead of print. PMID: 34459525. • P Bergman et al. (2021) “Safety and efficacy of the mRNA BNT162b2 vaccine against SARS-CoV-2 in five groups of immunocompromised patients and healthy controls in a prospective open-label clinical trial.” EbioMedicine, in press • W.Zhong et al. (2021) “Next generation plasma profiling of COVID-19 patients with mild and moderate symptoms”[ EbioMedicine, in press Technology development for viral detection and analysis • S Mravinacova. et al., (2021) A cell-free high throughput assay for assessment of SARS-CoV-2 neutralizing antibodies.” New Biotechnology 66, 46. • SM Mangsbo et al. (2021) An evaluation of a FluoroSpot assay as a diagnostic tool to determine SARS-CoV-2 specific T cell responses, PLOS One 16 (9), e0258041 • N. Kharlamova et al. (2021) "False Positive Results in SARS-CoV-2 Serological Tests for Samples From Patients With Chronic Inflammatory Diseases," Frontiers in Immunology, 12 (1365) 666114) • S. Hober et al. (2021) "Systematic evaluation of SARS-CoV-2 antigens enables a highly specific and sensitive multiplex serological COVID-19 assay," Clinical and Translational Immunology 10 (7) e1312 • N. Roxhed et al (2021) Multianalyte serology in home-sampled blood enables an unbiased assessment of the immune response against SARS-CoV-2. Nat Commun. 12(1):3695. • S. Hober et al (2021) “Rapid and sensitive detection of SARS-CoV-2 infection using quantitative peptide enrichment LC-MS/MS analysis” eLife, in press Clinical studies • A.-S. Rudberg et al. (2020) "SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden.," Nature Communications, 11(1) 5064. • S. Havervall et al. (2021) "Antibody responses after a single dose of ChAdOx1 nCoV-19 vaccine in healthcare workers previously infected with SARS-CoV-2," EBioMedicine, 70, 103523 • J. Dillner et al., (2021) "Antibodies to SARS-CoV-2 and risk of past or future sick leave," Scientific Reports, 11 (1), 5160 • G. Alkurt et al (2021) G “Seroprevalence of coronavirus disease 2019 (COVID-19) among health care workers from three pandemic hospitals of Turkey” PLoS One 16(3): e0247865. • B. Keskinkiliç et al (2021) ”A Resilient Health System in Response to Coronavirus Disease 2019: Experiences of Turkey” Front Public Health. 2021 8:577021. • K. A. Högelin et al.(2021) "Development of humoral and cellular immunological memory against SARS-CoV-2 despite B cell depleting treatment in multiple sclerosis," iScience, 24 (9) 103078 • J. Dillner et al. (2021) "High Amounts of SARS-CoV-2 Precede Sickness Among Asymptomatic Health Care Workers," The Journal of Infectious Diseases, 224 (1), 14-20. • H. Alkharaan et al. (2021) "Persisting Salivary IgG Against SARS-CoV-2 at 9 Months After Mild COVID-19 : A Complementary Approach to Population Surveys," Journal of Infectious Diseases, 224 (3), 407. • S. Klevebro et al. (2021) "Risk of SARS-CoV-2 exposure among hospital healthcare workers in relation to patient contact and type of care," Scandinavian Journal of Public Health. 49 (7), 707-712 • S. Hassan et al.(2021) "SARS-CoV-2 infections amongst personnel providing home care services for older persons in Stockholm, Sweden," Journal of Internal Medicine, 290 (2), 430-436. • S. Havervall et al. (2021) "Symptoms and Functional Impairment Assessed 8 Months After Mild COVID-19 Among Health Care Workers," Journal of the American Medical Association (JAMA), 325, 2015. • W. Zhong et al. (2021) "Next generation plasma proteome profiling of COVID-19 patients with mild to moderate symptoms" EBioMedicine. In Press. Therapeutic development • O. Altay et al (2021) “Combined Metabolic Activators Accelerates Recovery in Mild-to-Moderate COVID-19” Advance Science (Weinh). 2021 8(17):e2101222. • O. Altay et al (2020) “Current Status of COVID-19 Therapies and Drug Repositioning Applications” iScience. 23(7):101303. In summary, the Human Protein Atlas consortium has used their knowledge, technology platforms and resources to aid in the fight towards the pandemic. This includes technology development, viral assay optimizations, basic biology research, community-based research as well as diagnostic and drug development. SARS-CoV-2 related proteinsBelow is a summary of the tissue and cell expression patterns of known SARS-CoV-2 interacting human proteins, based on transcriptomics and antibody-based proteomics. If you have a suggestion for other human proteins to include here, please send an email to contact@proteinatlas.org SARS-CoV-2 entry receptors: ACE2 For more information about ACE2 and its cell type-specific expression in human tissues, also see: Hikmet F et al. (2020) SARS-CoV-2 entry associated proteases: TMPRSS2, CTSB, CTSL SARS-CoV-2 interacting proteins: Human proteins interacting with SARS-CoV-2 according to Gordon DE et al. (2020)
|
The Project
The Human Protein Atlas

 MENU
MENU